- Research
- Open access
- Published:
Systematic literature review of pharmacists in general practice in supporting the implementation of shared care agreements in primary care
Systematic Reviews volume 11, Article number: 88 (2022)
Abstract
Background
Rising demand for healthcare continues to impact all sectors of the health service. As a result of the growing ageing population and the burden of chronic disease, healthcare has become more complex, and the need for more efficient management of specialist medication across the healthcare interface is of paramount importance. With the rising number of pharmacists working in primary care in clinical roles, is this a role that pharmacists could support to ensure the successful execution of shared care agreement (SCA) in primary care for these patients?
Aim of the review
Systematic review to identify activities and assess the interventions provided by pharmacists in primary care on SCA provision and how it affects health-related quality of life (HRQoL) for patients.
Method
Primary studies in English which tested the intervention or obtained views of stakeholders related to pharmacist input to shared care agreement within primary care were included. The following electronic databases were systematically searched from the date of inception to November 2021: AMED®, CINAHL®, Cochrane Database of Systematic Reviews (CDSR), EMBASE®, EMCARE®, Google Scholar, HMIC®, MEDLINE®, PsycINFO®, Scopus and Web of Science®. Grey literature sources were also searched. The search was adapted according to the respective database-specific search tools. It was searched using a combination of Medical Subject Heading terms (MeSH), free-text search terms and Boolean operators.
Results
A total of 5244 titles/abstracts were screened after duplicates were removed, and 64 full articles were assessed for eligibility. On examination of full text, no studies met the inclusion criteria for this review.
Conclusion
This review highlights the need for further research to evaluate how pharmacists in general practice can support the safe and effective integration of specialist medication in primary care with the use of SCA.
Systematic review registration
NIHR PROSPERO No: 2020 CRD42020165363.
Introduction
Healthcare systems in the world are facing significant challenges as a result of severe funding pressure, a growing ageing population, societal changes, rising demand and a limited supply of some healthcare professional groups [1,2,3]. This is compounded by the increasing prevalence of long-term conditions (LTC), in particular, people having two or more conditions which are being supported by different parts of the healthcare system [4]. The UK is home to the National Health Service (NHS), one of the largest healthcare systems in the world. In the UK, LTCs account for 70% of the NHS healthcare budget [4]. With the continued demands in the NHS, the current models of dealing with long-term conditions are not sustainable; the need to innovate in order to continue to deliver world-class healthcare outcomes within a limited financial envelope is critical [5]. Care needs to be provided in the right place and at the right time to ensure that the healthcare system meets the current and future needs of a nation’s healthcare provision [6]. In response to this new normal, care must not be fragmented between healthcare systems, e.g. pre-hospital, hospital and specialist care [7].
This is of particular importance in countries where healthcare systems are well developed where care needs to move seamlessly from the gatekeeping primary care systems to the hospital and specialist services for the benefit of patient care [8]. Effective communication and cooperation between primary and secondary care are critical to making the best use of limited resources [9] and to ensure the patient receives high-quality joined-up care [8, 10, 11]. A tool that has been used in the literature to support effective integrated care between primary and secondary care is the shared care agreement (SCA) [12,13,14]. The SCA was designed to provide a framework for the seamless sharing of care and to facilitate the passage of hospital-prescribed medication or a consultant-managed patient into primary care.
The term shared care agreement has various definitions, none of which is universally agreed on [14,15,16,17,18]. The primary description to describe shared care was by Hickman et al. in their seminal paper on the taxonomy of shared care in 1994 [15]. The original definition of shared care described shared care as The joint participation of general practitioners and hospital consultants in the planned delivery of care for patients with chronic inflammatory musculoskeletal disorders, informed by an enhanced information exchange over and above the routine clinic, discharge and referral letters [15]. A more recent evolved definition describes these arrangements as the joint participation of primary and speciality care practitioners in the planned delivery of care for patients with a chronic condition, informed by enhanced information exchange, over and above routine discharge and referral notices [16]. This evolved definition takes into account the changes in primary care since the primary definition was described.
Since the introduction of an executive letter EL (91) 127 by the NHS in 1991 described SCA to support prescribing between hospitals and GPs [19], several problems have marred the integration of SCA into primary care, and in 2017, the British Medical Association (BMA) stated that shared care is still not working effectively [20]. General practitioners have expressed concern about poor communication between primary and secondary care, lack of follow-up and monitoring and the medico-legal responsibilities for the prescriber when they accept shared care [16, 21,22,23]. After 30 years, EL (91) 127 has been superseded by the new national guidance released in 2018 for England [24]. The guidance was designed to overcome the challenges of shared care that have been exhibited in the healthcare system over the last 30 years [21]. The document has described a role for the pharmacist in general practice in supporting joint working and collaboration to ensure that primary care prescribers have access to information on new or less familiar medicines and how they can support the introduction of medicines into primary care [21]. Evidence indicates that pharmacists have a significant role in medicine optimisation and improving safe and effective medication use in primary care [25]. In addition, the literature has shown that pharmacists in general practice are increasingly playing a central role in managing medicines [26], such as setting up systems for safe monitoring and prescribing high-risk medicines such as direct oral anticoagulants, lithium, non-steroidal anti-inflammatory drugs (NSAIDs) prescribing and medicine safety requirement in general practice. With the support of government initiatives to increase the number of pharmacists in general practice to support new models of care, the pharmacist could be seen as a vital component in bridging the transfer of care from secondary to primary care settings [4, 27, 28]. This paper aims to review the literature on the role of a pharmacist in general practice with regard to SCA support, their roles and identify the potential benefits, barriers and facilitators to their potential integral role.
Aim of the review
This study aimed to identify activities and assess the interventions provided by pharmacists in primary care on SCA provision. The specific objectives were to determine the following:
-
The types of interventions/activities being provided by pharmacists in supporting SCA in a general practice setting
-
The effectiveness of these interventions/activities on health-related quality of life (HRQoL) for patients, to consider the impact of clinical pharmacist supporting shared care agreement in a general practice setting.
Method
Study registration
The review protocol was registered with the International Prospective Register for Systematic Review (PROSPERO database; registration number CRD42020165363). The review was guided by the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions [29]. The reporting of the review complies with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement and checklist (refer to supplementary information S2 and S3) [30].
Eligibility criteria for study inclusion
The search was focused on locating studies eligible for inclusion or excluded based on the criteria below.
Inclusion criteria
The following are the inclusion criteria:
-
1.
Only primary studies (qualitative, quantitative and mixed studies)
-
2.
Studies which have tested an intervention and/or have obtained views of stakeholders (pharmacists, GPs, medical specialists, practice staff and patients) related to SCA in the primary care setting
-
3.
Studies in which a pharmacist has input within a primary care setting to provide non-dispensing care
Exclusion criteria
The following are the exclusion criteria:
-
1.
Studies in which the intervention has been provided only in secondary or tertiary care settings (hospitals, specialist clinics and national and regional specialist centre)
-
2.
Studies written in a language other than English
-
3.
Studies presented as editorials, protocols and commentaries
Information sources and search strategy
Specific search strategies were developed with expert information specialists and included broad and narrow, free-text and thesaurus-based terms. The term pharmacist was used as a general term to allow greater scope to find multiple roles provided by pharmacists, which included prescribers. Boolean operators and truncation were used to ensure we maximised our search strategy. The following eleven databases were systematically searched from date of inception to November 2021: Allied and Complementary Medicine Database (AMED®) (1985 to 07.11.2021) Platform: Ovid®; Cumulative Index to Nursing and Allied Health Literature (CINAHL®) (1950 to 07.11.2021) Platform: EBSCO®; Cochrane Database of Systematic Reviews (CDSR) (accessed on 07.11.2021) Platform: Wiley® online library; Excerpta Medica database (EMBASE®) (1974 to 07.11.2021) Platform: Ovid®; EMCARE® (1995 to 07.11.2021) Platform: Ovid®; Google Scholar (accessed on 07.11.2021) Platform: Google UK®; Healthcare Management Information Consortium (HMIC®) (1979 to November 2021) Platform: Ovid®; Medical Literature Analysis and Retrieval System Online (MEDLINE®) (1946 to 07.11.2021) Platform: Ovid®; PsycINFO®, Psychology and Behavioural Sciences Collection, Health Business Elite, Biomedica Reference Collection: Comprehensive Library, Information Science & Technology Abstracts (1967 to 07.11.2021) Platform: EBSCOhost®; and Scopus (2004 to 07.11.2021) Platform: Elsevier, Web of Science® Core Collection (1970-07.11.2021) Platform: Clarivate Analytics®. The search was adapted according to the respective database-specific search tools. It was searched using a combination of Medical Subject Heading terms (MeSH) where available, free-text search terms and Boolean operators. Refer to supplementary information S1 ‘Search terms’ for the specific detail of the search used for each database. Search results in languages other than English were noted, but for practical reasons, only search results in English or translated into English were included in this review. In an effort to identify unpublished studies, a search of grey literature was performed (http://www.opengrey.eu/ on 07.11.2021) to identify studies not indexed in the databases listed above. The term grey literature in this paper refers to sources used to describe a wide range of information produced outside of traditional publishing and distribution channels and which is often not well represented in indexing databases.
Data collection and analysis
All references from database search were downloaded into EndNote® X8.2 [31] reference manager, which was used to collate and remove duplicate records, to screen titles and abstracts and to store the full text of retrieved studies. Citations from OpenGrey could not be uploaded to EndNote® reference manager and therefore were uploaded to a Microsoft Excel® 2016 spreadsheet. Duplicate citations were removed by the automatic de-duplicating option in EndNote®X8.2 and were supplemented by hand-searching. Two researchers (NI and CH) examined the titles and abstracts of all eligible articles according to the inclusion and exclusion criteria listed above. References to be screened were allocated into groups and was divided into ‘include’, ‘exclude’ and ‘potential’ groupsets. The full-text articles of any abstracts classified as potentially meeting the inclusion criteria were retrieved and analysed independently by two authors (NI and CH) against the predefined inclusion and exclusion criteria with differences between reviewers resolved by consensus. The principal authors of all included papers were contacted to explore the potential for any studies considered vital to them that may have been missed in the search strategy. A data extraction form from the Cochrane collaboration was utilised to extract data from eligible papers [32]. Raw data from quantitative studies were extracted onto Microsoft Excel® 2016 spreadsheet. If data could not be pooled for meta-analysis, the plan was to undertake a narrative synthesis of results. The qualitative data synthesis methodology was decided upon after the quantity, quality, conceptual richness, and contextual thickness of the qualitative studies were determined. The intended results and data synthesis were to be conducted by authors NI and CH independently to assure the data extraction integrity.
The Mixed Method Appraisal Tool (MMAT) 2018 version was used to appraise and describe the methodological quality of included quantitative, qualitative and mixed-method studies. A pilot test of two articles was conducted to ensure consistent interpretation between the two authors (NI and CH). Discrepancies were resolved through discussion and consensus with the research team. If further information was required to appraise a particular study, an attempt was made to contact the authors by phone or email. Quality scores will be calculated using the MMAT tool. However, this did not solely determine if studies were of “low” or “high” quality, as a descriptive summary using MMAT criteria was considered [33]. If a study received a low score, it was compared with those with a higher score (higher quality studies) to consider if this modifies the outcome and interpretation of our synthesis.
Results
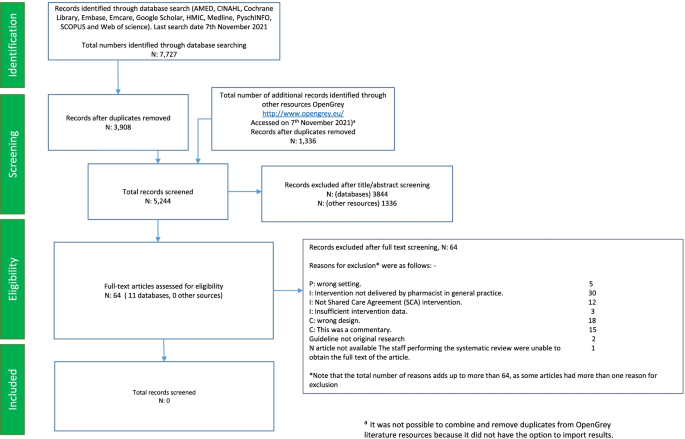
The database search yielded 7727 citations. After duplicates were removed, the database search identified 3908 citations. Based on the title and abstract information, 3844 citations were ‘excluded’, leaving 64 citations identified as ‘potentially relevant’ articles requiring a full-text article text review. In addition to the 3908 citations that were yielded by the databases, 1336 additional citations were retrieved from http://www.opengrey.eu/ and were screened separately as they could not be uploaded onto EndNote® X8.2 [31] reference manager. After screening, no pertinent articles that met the inclusion and exclusion criteria were extracted from grey literature sources.
On the examination of the full text of the 64 studies in the ‘potentially relevant’ category, no publications addressing evidence to identify activities and to assess interventions provided by pharmacists in primary care on SCA provision were identified (see Table 1, which includes a tabulated list of the 64 excluded studies along with reasons for exclusion, with some articles having more than one reason for exclusion). Out of the 64 excluded studies, one study (a conference proceeding) could not be found, and an attempt was made to contact the author to obtain further information (full set of results). The author did not respond; hence, this article was excluded from our review as the reviewers could not assess the eligibility based on the information from the abstract. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) flow chart (Fig. 1) shows the identification, screening and selection of papers for this review. There were no included studies for which to assess the risk of bias or to apply for evidence synthesis.
Discussion
This paper aimed to systematically assess the pharmacist’s role in general practice in supporting the implementation of SCA in primary care. No articles met our inclusion criteria. Several studies have tried to define the role of pharmacists in general practice, but the working definition has not been defined by healthcare organisations or the research community [98, 99]. Another reason for there to be no studies available is because the GP pharmacist’s role is still a relatively new role in healthcare and little existing literature in role evolution is available [100].
Comparison with other studies
There is an agreement in the literature that the pharmacist role is developing at pace within the general practice setting and recent international systematic reviews and meta-analyses demonstrate positive effects on medication use and clinical outcomes [99, 101]. Pharmacists integrated into general practice teams can perform a variety of roles. This includes direct patient care, medicines reconciliation and education to members of the healthcare team and in the detection and resolution of medication-related problems [102,103,104]. A recent review of the impact of integrating pharmacists into primary care teams on health systems indicators on healthcare utilisation by Hayhoe et al. did highlight the activities provided by pharmacists in general practice. Still, it failed to discover activities to support SCA in the published literature [105]. Internationally, other terminologies and contexts vary, giving one example being collaborative care agreements by Stuhec et al. in Slovenia [106,107,108,109]. The focus has been aimed in this international context as clinical pharmacists share a role within their own heterogeneous setting and sharing this with various physicians in managing a patient with chronic conditions, not necessarily in the same setting such as GP surgery in the UK where the GP is seen anecdotally as the main gatekeeper and first point of contact for all medication issues related to the patient. The observational studies by Stuhec et al. have focused on older patient and psychiatric patients. Further research would be required to homogenise and formalise an internationally recognised term for shared care agreements.
The most recent Cochrane systematic review, which assessed the effectiveness of shared care across the interface between primary and speciality care in the management of long-term conditions, did not consider models of integrating care between pharmacists and primary care physicians [18]. The authors of the Cochrane review stated that this limited its generalisability to all types of collaborative care due to the contextual specificity. The review did note that several other models of shared or collaborative care should be considered for review. This systematic review has highlighted that the model of care involving a pharmacist in primary care supporting SCA is not currently present in the literature and should be considered for further investigation.
Implications of the review findings on clinicians and decision-makers in healthcare and future studies
The changing needs of the population make it increasingly important that the patient’s multiple needs are met in a well-coordinated way. To respond effectively to these changing needs, healthcare teams need to utilise the skills available across our healthcare teams. To help alleviate these pressures, it has been recommended that the NHS should maximise the opportunities offered by pharmacists [9, 110, 111]. Pharmacists can take on significant amounts of work currently done by GPs and other staff in general practice [111]. To explore whether shared care management could be implemented successfully by the pharmacist in general practice, we need to understand the relevant and important pharmacist related barriers and facilitators concerning the implementation of this role. The influence of these factors needs to be recognised and considered and how this can inform further research into this area.
Decision-making
Collaboration between pharmacists and the healthcare team is of paramount importance, and understanding the skills of multiple healthcare professionals will help support an integrated system [112]. We need to understand the role in which pharmacists will support SCA and how general practitioners are willing to integrate pharmacists within this process. A finding from earlier research has shown that general practice has a positive experience of pharmacist recommendations in a range of conditions [113,114,115]. However, how would this apply to SCA when patients and healthcare staff need to understand the role of the pharmacist and agree to the SCA? Would patients accept pharmacists undertaking this new role within the general practice?
Funding and workload
General practice continues to be concerned with the inappropriate funding associated with supporting shared care medication [21]. Commissioners have always stated that the funding of specialist’s drugs has been agreed so cost should not be an issue. General practitioners have expressed concerns that the additional workload required to support the integration of specialised medication is a factor they believe has not been appreciated [116]. This has been exacerbated by the COVID-19 pandemic, which has seen a rise in how general practice is expected to manage care which would typically be carried out in a hospital setting which in turn has contributed to a growing workload in primary care [117]. Previous studies have suggested that the impact of practice-based pharmacists will not be on workload but quality and safety [118]. It is reasonable to ask whether GPs would support pharmacists taking on this role without appropriate funding and whether this intervention will reduce workload in general practice.
Working definition and liability
We need to consider a working definition of the practice pharmacist role in shared care. The differences in pharmacists’ primary care roles have been identified in the international literature. The lack of clarity and knowledge of this primary care role can negatively affect their potential integration into the primary care team [119]. The knowledge, skills and attitudes required to support SCA should be made readily available to practice pharmacists, primary care teams and the general public. This would enable SCA management to be developed and applied nationally across primary care. The rapid emergence of new professional roles for pharmacists also means that arrangement in respect of liability needs to keep up with the changing nature of pharmacy practice within this more complex intervention.
This empty review can act as a platform to inform policymakers in healthcare that there is a lack of robust evidence that evaluates the role and potential value of pharmacists supporting SCA in general practice. Healthcare systems must seek out the best possible evidence to support patients within this new healthcare environment. However, the absence of research in this area does not justify the rejection of this intervention [120]. As the role is relatively new, there is still work to be done to develop the evidence base of pharmacists working in general practice to support SCA and the benefits of this role within the healthcare system.
Limitations
A limitation of this review is that the search strategy included a literature search of articles only in the English language. Other articles may have been published on pharmacists supporting SCA in general practice in non-English journals. Personal commentaries, blogs and opinion pieces were excluded from this systematic review due to the research design. This may have excluded observations that are occurring in general practice but have not been critically appraised. Another limitation is that the term SCA may be used as an alternate term from an international perspective. Despite the use of 12 healthcare-related bibliographical databases and the extensive use of keywords to maximise the sensitivity of relevant studies, after removal of duplicates, this yielded a low number of citations of titles and abstracts, another limitation. This systematic review used database word stock to establish standard search terms; however, it cannot be discounted that this may not have retrieved all articles relating to this intervention. Another limitation that needs to be considered is that abstracts from conference proceedings were not included in the synthesis, which could account for the empty return due to the high evidence bar for the systematic review.
Conclusion
This systematic review identified no eligible studies on the interventions provided by a pharmacist in supporting SCA in general practice. It is not possible to formulate what the role pharmacists can play in supporting SCA in general practice based on scientific evidence. There is an urgent need for studies that identify, observe and evaluate GP-based pharmacists’ roles concerning SCA that currently occur in clinical practice. Comparing and contrasting each general practice’s approach will ensure the development of a consensus for the role of GP pharmacists on SCA based on the current SCAs occurring in general practice, and how to implement this intervention consistently. The role of the pharmacist is expanding in general practice, and interventions which prove beneficial for patients and the healthcare system are required to meet the ever-changing demand in healthcare and to ensure that these new interventions follow the evidence. This empty systematic review serves as a starting point for further clinical research in this area.
Abbreviations
- SCA:
-
Shared care agreement
- HRQoL:
-
Health-related quality of life
- MeSH:
-
Medical Subject Heading terms
- LTC:
-
Long-term conditions
- NHS:
-
National Health Service
- BMA:
-
British Medical Association
- PRISMA:
-
Preferred Reporting Items for Systematic Review and Meta-Analysis
- MMAT:
-
Mixed Method Appraisal Tool
References
High-level commission on health employment and economic growth. Working for health and growth: investing in the health workforce. World Health Organization. 2016. http://apps.who.int/iris/bitstream/handle/10665/250047/9789241511308-eng.pdf?sequence=1. Accessed 03 Aug 2020.
United Nations Department of Economic and Social Affairs, Population Division. World population ageing 2019 (ST/ESA/SER.A/444): United Nations; 2020. https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/files/documents/2020/Jan/un_2019_worldpopulationageing_report.pdf. Accessed 03 Aug 2020
Campbell J, Dussault G, Buchan J, Pozo-Martin F, Guerra Arias M, Leone C, et al. A universal truth: no health without a workforce. Forum Report 2013, Third Global Forum on Human Resources for Health, Recife, Brazil. Geneva: Global Health Workforce Alliance and World Health Organization; 2013. https://www.who.int/workforcealliance/knowledge/resources/GHWA-a_universal_truth_report.pdf?ua=1. Accessed 10 Aug 2020
NHS England, Public Health England, Care Quality Commission, Monitor, NHS Trust Development Authority, Health Education England. NHS five year forward view: NHS England; 2014. https://www.england.nhs.uk/ourwork/futurenhs/. Accessed 10 Aug 2020
Rosen R. Delivering general practice with too few GPs: Nuffield Trust; 2019. https://www.nuffieldtrust.org.uk/files/2019-10/general-practice-without-gps-v2.pdf. Accessed 14 Aug 2020
Jones R, Jones R, Newbold M, Reilly J, Drinkwater R, Stoate H. The future of primary and secondary care. Br J Gen Pract. 2013;63:379–82. https://doi.org/10.3399/bjgp13X669400.
Scally G, Jacobson B, Abbasi K. The UK’s public health response to covid-19. BMJ. 2020. https://doi.org/10.1136/bmj.m1932.
Sampson R, Cooper J, Barbour R, Polson R, Wilson P. Patients’ perspectives on the medical primary-secondary care interface: systematic review and synthesis of qualitative research. BMJ Open. 2015. https://doi.org/10.1136/bmjopen-2015-008708.
Naylor C, Alderwick H, Honeyman M. Acute hospitals and integrated care: from hospitals to health systems: King’s Fund; 2015. https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/acute-hospitals-and-integrated-care-march-2015.pdf. Accessed 26 Aug 2020
Cresswell A, Hart M, Suchanek O, Young T, Leaver L, Hibbs S. Mind the gap: improving discharge communication between secondary and primary care. BMJ Qual Improv Rep. 2015. https://doi.org/10.1136/bmjquality.u207936.w3197.
Epstein RM. Communication between primary care physicians and consultants. Arch Fam Med. 1995;4:403–9.
Drummond N, Abdalla M, Buckingham JK, et al. Integrated care for asthma: a clinical, social, and economic evaluation. Grampian asthma study of integrated care (GRASSIC). BMJ. 1994;308:559–64. https://doi.org/10.1136/bmj.308.6928.559.
Integrated care for diabetes: a clinical, social and economic evaluation. Diabetes integrated care evaluation team. BMJ. 1994;308:1208–12. https://doi.org/10.1136/bmj.308.6938.1208.
Midlands Therapeutics Review and Advisory Committee. Independent review of medicines for primary care. http://ccg.centreformedicinesoptimisation.co.uk/mtrac/. Accessed 03 Aug 2020.
Hickman M, Drummond N, Grimshaw J. A taxonomy of shared care of chronic disease. J Public Health Med. 1994;16:447–54.
Horne R, Mailey E, Frost S, Lea R. Shared care: a qualitative study of GPs’ and hospital doctors’ views on prescribing specialist medicines. Br J Gen Pract. 2001;51:187–93.
Specialist Pharmacy Service. RMOC work programme: NHS England; 2020. https://www.sps.nhs.uk/topics/?with=rMOc. Accessed 03 Mar 2020
Smith SM, Cousins G, Clyne B, Allwright S, O’Dowd T. Shared care across the interface between primary and specialty care in management of long term conditions. Cochrane Database Syst Rev. 2017. https://doi.org/10.1002/14651858.CD004910.pub3.
National Health Service Management Executive. Responsibility for prescribing between hospitals and GPs. London: NHS Management Executive; 1991.
British Medical Association. Primary and secondary care interface guidance. https://www.bma.org.uk/collective-voice/committees/general-practitioners-committee/gpc-current-issues/nhs-england-standard-hospital-contract-guidance-2017-2019/primary-and-secondary-care-interface-guidance. Accessed 03 Mar 2020.
Shared care protocols – have they had their day? Drug Ther Bull. 2017;55:133 https://dtb.bmj.com/content/55/12/133. Accessed 03 Mar 2020.
Wilcock M, Rohilla A. Three decades of shared care guidelines: are we any further forward? Drug Ther Bull. 2020; https://dtb.bmj.com/content/58/5/67. Accessed 03 Mar 2020.
Crowe S, Cantrill JA, Tully MP. Shared care arrangements for specialist drugs in the UK: the challenges facing GP adherence. Qual Saf Health Care. 2010. https://doi.org/10.1136/qshc.2009.035857.
NHS England. Responsibility for prescribing between primary & secondary/tertiary care; 2018. https://www.england.nhs.uk/publication/responsibility-for-prescribing-between-primary-and-secondary-tertiary-care/. Accessed 03 Aug 2020
Tan EC, Stewart K, Elliott RA, George J. Pharmacist services provided in general practice clinics: a systematic review and meta-analysis. Res Soc Adm Pharm. 2014:608–22. https://doi.org/10.1016/j.sapharm.2013.08.006.
Wood S. Safer prescribing and monitoring of high-risk medicines. Prescriber. 2020;31(4):10–5.
NHS. The NHS long term plan; 2019. https://www.longtermplan.nhs.uk/. Accessed 03 Mar 2020
Petty D. Clinical pharmacist roles in primary care networks. Prescriber. 2019;30(11):22–6.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane; 2019. https://training.cochrane.org/cochrane-handbook-systematic-reviews-interventions. Accessed 05 May 2020.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009. https://doi.org/10.1136/bmj.b2535.
Clarivate Analytics. EndNote. Version X8.2. Philadelphia: Clarivate Analytics; 2018.
Cochrane Effective Practice and Organisation of Care (EPOC). Data collection form. In: EPOC Resources for review authors: Cochrane; 2017. https://epoc.cochrane.org/resources/epoc-resources-review-authors. Accessed 04 Mar 2020.
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed Methods Appraisal Tool (MMAT), version 2018. Registration of Copyright (#1148552), Canadian Intellectual Property Office, Industry Canada. Available at: - http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf. Accessed 12 April 2022
Adams B. NHS alliance: The evolution of primary care. Prescriber. 2015;26(3):32–4. Available: - https://wileymicrositebuilder.com/prescriber/wpcontent/uploads/sites/23/2015/12/NHS-Alliance-the-evolution-of-primary-care.pdf. Accessed 12 Apr 2022.
Agyapong VI, Conway C, Guerandel A. Shared care between specialized psychiatric services and primary care: the experiences and expectations of consultant psychiatrists in Ireland. Int J Psychiatry Med. 2011;42(3):295–313. https://doi.org/10.2190/2FPM.42.3.e.
Al-Alawi K, Al Mandhari A, Johansson H. Care providers' perceptions towards challenges and opportunities for service improvement at diabetes management clinics in public primary health care in Muscat, Oman: a qualitative study. BMC Health Serv Res. 2019;19(1). https://doi.org/10.1186/s12913-019-3866-y.
Alhabib S, Aldraimly M, Alfarhan A. An evolving role of clinical pharmacists in managing diabetes: Evidence from the literature. Saudi Pharm J. 2016;24(4):441–6. https://doi.org/10.1016/j.jsps.2014.07.008.
Ali S, Smith TL, Mican L, Brown C. Psychiatric providers' willingness to participate in shared decision-making when prescribing psychotropic medications. J Pharm Pract. 2013;26(3):334. https://doi.org/10.1177/2F8755122515578288.
Aljumah K, Hassali MA. Impact of pharmacist intervention on adherence and measurable patient outcomes among depressed patients: A randomised controlled study. BMC Psychiatry. 2015;15(1). https://doi.org/10.1186/s12888-015-0605-8.
Almunef M, Mason J, Curtis C, Jalal Z. Management of chronic illness in young people aged 10-24 years: A systematic review to explore the role of primary care pharmacists. Arch Dis Child. 2019;104(7):e2.39–e2. https://doi.org/10.1136/archdischild-2019-nppc.44.
Alshehri AA, Cheema E, Yahyouche A, et al. Evaluating the role and integration of general practice pharmacists in England: a cross-sectional study. Int J Clin Pharm. 2021;43:1609–18. https://doi.org/10.1007/s11096-021-01291-6.
Anderson K, Freeman C, Rowett D, Burrows J, Scott I, Rigby D. Polypharmacy, deprescribing and shared decision-making in primary care: the role of the accredited pharmacist. J Pharm Pract. 2015;45(4):446–9. https://doi.org/10.1002/jppr.1164.
General Practitioner/pharmacy interface a local initiative Pharm J. 1994;253(6812):574.
The role of pharmacists in primary care groups (PCGs): a strategic approach. Pharm J. 1999;262(7038):445–6.
Pharmacy in a new age: the role of government. Pharm J. 1995;255(6863):1995.
Shared care addiction scheme starts. Pharm J. 2003;270(7252):782.
Ashcroft DM, Clark CM, Gorman SP. Shared care: A study of patients’ experiences with erythropoietin. Int J Pharm Pract. 1998;6(3):145–9. https://doi.org/10.1111/j.2042-7174.1998.tb00930.x.
Bains S, Naqvi M, West A. S126 The pharmacist-led accelerated transfer of patients to shared care for the monitoring and prescribing of immunomodulatory therapy during covid-19. Thorax. 2021;76:A75. https://thorax.bmj.com/content/76/Suppl_1/A75.2.
Bajramovic J, Emmerton L, Tett SE. Perceptions around concordance–focus groups and semi-structured interviews conducted with consumers, pharmacists and general practitioners. Health Expect. 2004;7(3):221–34. https://doi.org/10.1111/j.1369-7625.2004.00280.x.
Barnes E, Ashraf I, Din A. New roles for clinical pharmacists in general practice. Prescriber. 2017;28(4):26–9. https://wileymicrositebuilder.com/prescriber/wpcontent/uploads/sites/23/2017/04/Pharmacist-new-roles-EB-edit-AC-made-lsw.pdf.
Bellingham C. How to improve medicines management at the primary/secondary care interface. Pharm J. 2004;272(7287):210–1.
Berendsen AJ, de Jong GM, Meyboom-de Jong B, Dekker JH, Schuling J. Transition of care: experiences and preferences of patients across the primary/secondary interface–a qualitative study. BMC Health Serv Res. 2009;9(1):62. https://doi.org/10.1186/1472-6963-9-62.
Bojke C, Philips Z, Sculpher M, et al. Cost-effectiveness of shared pharmaceutical care for older patients : RESPECT trial findings. Br J Gen Pract. 2010;60(570):e20–7. https://doi.org/10.3399/bjgp09X482312.
British National Association of Health and Trusts. NAHAT Update: asthma care - the challenge ahead. Conference 1994.
Cain RM, Cain RM. The physician-pharmacist interface in the clinical practice of pharmacy. Ann Pharmacother. 2006;40(12):2240–2. https://doi.org/10.1345/aph.140048.
Carrington I, McAloon J. Why shared-care arrangements for prescribing in attention deficit hyperactivity disorder may not be accepted. Eur J Hosp Pharm. 2018;25(4):222–4.
Chana N, Porat T, Whittlesea C, Delaney B. Improving specialist drug prescribing in primary care using task and error analysis: an observational study. Br J Gen Pract. 2017;67(656):e157–67. https://doi.org/10.3399/bjgp17x689389.
Chartrand M, Maheu A, Guenette L, Martin E, Moisan J, Gregoire JP, Lauzier S, Blais L, Perreault S, Lalonde L. Implementation and evaluation of pharmacy services through a practice-based research network (PBRN). Journal of Population Therapeutics and Clinical Pharmacology. 2013;20(3):e272–3.
Cox WM. Evaluation of a shared-care program for methadone treatment of drug abuse: An international perspective. Journal of Drug Issues. 2002;32(4):1115–23. https://doi.org/10.1177/2F002204260203200407.
Crowe S, Tully MP, Cantrill JA. The prescribing of specialist medicines: what factors influence GPs’ decision making? Family practice. 2009;26(4):301–8.
Crowe S, Cantrill JA, Tully MP. Shared care arrangements for specialist drugs in the UK: the challenges facing GP adherence. Qual Saf Health Care. 2010;19(6):e54.
Duggan C, Beavon N, Bates I, Patel S. Shared care in the UK: Failings of the past and lessons for the future. Int J Pharm Pract. 2001;9(3):211–6. https://doi.org/10.1111/j.2042-7174.2001.tb01051.x.
Fearne J, Grech L, Inglott AS, Azzopardi LM. Development and evaluation of shared paediatric pharmaceutical care plan. Int J Clin Pharm. 2018;40(1):263–4.
Finch E, Ford C [ed]. Shared care at the primary and secondary interface: GPs and specialist drug services. Drug misuse and community pharmacy 2002 1st Edition. eBook ISBN 9780429229848.
Grixti D, Vella J, Fearne J, Grech L, Pizzuto MA, Serracino-Inglott A. Development of shared care guidelines in rheumatology. Int J Clin Pharm. 2014;36(4):850.
Gu Y, Humphrey G, Warren J, Tibby S, Bycroft J, editors. An Innovative Approach to Shared Care–New Zealand Pilot Study of a Technology-enabled National Shared Care Planning Programme. Health Informatics New Zealand Conference; 2012
James O, Cardwell K, Moriarty F, Smith SM, Clyne B, on behalf of the General Practice Pharmacist (GPP) Study Group. Pharmacists in general practice: a qualitative process evaluation of the General Practice Pharmacist (GPP) study. Family Practice. 2020;37(5):711–8. https://doi.org/10.1093/fampra/cmaa044.
Johnson C. Adult attention deficit and hyperactivity disorder (ADHD) clinic: A collaboration between psychiatry, primary care and pharmacy to improve access, care experience and affordability. JACCP. 2018;1(2):318.
Jones BW, Clark W. Shared care agreements - How to overcome the blank page. Pharm J. 2003;270(7234):165–6.
Jones C, Robinson H, Trickey J, Rees D, Jolliffe V, Wood J, et al. UPDATE ON THE INTRODUCTION OF DOSE TAPERING TO MODERNIzE AND IMPROVE THE BIOLOGICS SERVICE IN A DISTRICT GENERAL HOSPITAL. Rheumatology. 2017;56(suppl_2):kex062.143. https://doi.org/10.1093/rheumatology/kex062.143.
Jones E, Cuevas OA. P12 An audit on the use and monitoring of azathioprine (aza) in a paediatric gastroenterology centre. could nhs england via specialist commissioning rules (nhs-e-spr) be affecting quality of care? Arch Dis Child. 2018;103:e2. https://adc.bmj.com/content/103/2/e2.14.
Lloyd LA, Breslin A, Jones J. An audit of methotrexate monitoring in primary care as part of a shared care agreement. Rheumatology. 2009;(1):i61.
MacLellan J, Shahmanesh M, Singh S, Morton J, Estcourt C, Asboe. Shared care: how can we do it? Findings from the BHIVA primary care project. British HIV Association BHIVA. Available at: https://www.bhiva.org/file/PsGAzexFTYXJy/Shared-Care.pdf. Accessed 12 Apr 2022.
Mercer K, Burns C, Guirguis L, Chin J, Dogba MJ, Dolovich L, et al. Physician and pharmacist medication decision-making in the time of electronic health records: Mixed-methods study. J Med Internet Res. 2018;20(9). https://doi.org/10.2196/humanfactors.9891.
Mercer K, Neiterman E, Guirguis L, Burns C, Grindrod K. “My pharmacist”: Creating and maintaining relationship between physicians and pharmacists in primary care settings. Res Social Adm Pharm. 2020;16(1):102–7. https://doi.org/10.1016/j.sapharm.2019.03.144.
McWilliams T, Morakinyo K. Shared care guideline for the use of Methylphenidate, Dexamfetamine, Lisdexamfetamine dimesylate & Atomoxetine for the management of Attention Deficit Hyperactivity Disorder (ADHD) in Adults (18-64years). East London NHS Foundation Trust; 2017. https://gp-website-cdnprod.s3.amazonaws.com/shared-care-downloads/1539870612-c9e7983bdf34a9c9dcc7f3063eada5e9.pdf. Accessed 12 April 2022.
Mousa Y, Kayyali R, Goldsmith C, Coughlan L, Cairns C, Evans C. Investigating the potential for improved management of patients with long term conditions through shared-care protocols. Pharmacy World and Science. 2009;31(4):502.
National Instititute of Health and Care excellence NICE) 2015. Transition between inpatient hospital settings and community or care home settings for adults with social care needs. NICE guideline [NG27]. https://www.nice.org.uk/guidance/ng27. Accessed 12 April 2022.
Nkansah N, Mostovetsky O, Yu C, Chheng T, Beney J, Bond CM, et al. Effect of outpatient pharmacists' nondispensing roles on patient outcomes and prescribing patterns. Cochrane Database Syst Rev. 2010(7). https://doi.org/10.1002/14651858.CD000336.pub2.
O'Halloran KA. Developing Integrated Care Teams Across the North West London System. Int J Integr Care. 2016;16(6):A150. https://doi.org/10.5334/ijic.2698.
Petty D. Clinical pharmacist roles in primary care networks. Prescriber. 2019;30(11):22–6. https://doi.org/10.1002/psb.1802.
Murphy K. Clozapine, concomitant medications and consumers: Assessing the accuracy of medication records and the lived experience of people prescribed clozapine under shared care arrangements. Thesis Masters. Australia: Griffith University Queensland; 2018. https://doi.org/10.25904/1912/162.
Richmond S, Morton V, Cross B, Wong ICK, Russell I, Philips Z, et al. Effectiveness of shared pharmaceutical care for older patients: RESPECT trial findings. Br J Gen Pract. 2010;60(570):e10–9. https://doi.org/10.3399/bjgp09X473295.
Roberts RI. The welsh sahred care prescribing project. Pharm J. 1997;258(6935).
Sibbald B, Wilkie P, Raftery J, Anderson S, Freeling P. Prescribing at the hospital-general practice interface. II: Impact of hospital outpatient dispensing policies in England on general practitioners and hospital consultants. BMJ. 1992;304(6818):31–4. https://doi.org/10.1136/bmj.304.6818.31.
Shemilt R, Azar M, Singh G, Campbell A, Gunnell KA. White S. An evaluation into the refusal of essential shared care agreements: Quetiapine. Pharmacoepidemiol Drug Saf. 2021;30(S2):3–20. https://doi.org/10.1002/pds.5315.
Smith SM, Cousins G, Clyne B, Allwright S, O'Dowd T. Shared care across the interface between primary and specialty care in management of long term conditions. Cochrane Database Syst Rev. 2017;2(2):CD004910. https://doi.org/10.1002/14651858.CD004910.pub3.
Sowerby C, Taylor D. Cross-sector user and provider perceptions on experiences of shared-care clozapine: a qualitative study. BMJ Open. 2017;28;7(9):e017183. https://doi.org/10.1136/bmjopen-2017-017183.
Steckowych K, Smith M. Lessons learned and real-world challenges of implementing clinical pharmacy services in a primary care office. J Am Pharm Assoc. 2018;58(3):e132–e3 4.
Swallow VM, Nightingale R, Williams J, et al. Multidisciplinary teams, and parents, negotiating common ground in shared-care of children with long-term conditions: A mixed methods study. BMC Health Serv Res. 2013;13:264. https://doi.org/10.1186/1472-6963-13-264.
Taylor D, Sutton J, Dawson H. User and staff perspectives of clozapine clinic services. Int J Pharm Pract. 2010;2:72.
Terry DRP. Medicines management acrosss the primary-hospital healthcare interface: a study of paediatric patients. PhD thesis. https://publications.aston.ac.uk/id/eprint/15825/. Accessed 12 Apr 2022.
Terry D, Sinclair A. Prescribing for children at the interfaces of care. Arch Dis Child Educ Pract Ed. 2012;97(4):152–6.
Travis SS, Bethea LS. Medication administration by family members of dependent elders in shared care arrangements. Journal of Clinical Geropsychology. 2001;7(3):231–43. https://doi.org/10.1023/A:1011395229262.
Tolley L, Azar M, Singh G, Gunnel KA, Campbell A, White S. An evaluation into the refusal of essential shared care agreements: Aripriprazole. Pharmacoepidemiol Drug Saf. 2021;30(S2):3–20. https://doi.org/10.1002/pds.5315.
Walker M. Shared care for opiate substance misusers in Berkshire. Pharm J. 2001;266(7144):547–52.
Yones E, Mullan J, Horwood A, Connell N, Odams S, Maloney J, et al. Prescribing dronedarone for paroxysmal atrial fibrillation: How is it done across the UK and is it safe? Eur J Hosp Pharm. 2019;26(4):220–2.
Butterworth J, Sansom A, Sims L, Healey M, Kingsland E, Campbell J. Pharmacists’ perceptions of their emerging general practice roles in UK primary care: a qualitative interview study. Br J Gen Pract. 2017;67(662):e650–8.
Tan EC, Stewart K, Elliott RA, George J. Pharmacist consultations in general practice clinics: the pharmacists in practice study (PIPS). Res Soc Adm Pharm. 2013:623–32. https://doi.org/10.1016/j.sapharm.2013.08.005.
Bradley F, Seston E, Mannall C, Cutts C. Evolution of the general practice pharmacist’s role in England: a longitudinal study. Br J Gen Pract. 2018;68(675):e727–34.
Hazen AC, De Bont AA, Boelman L, Zwart DL, et al. The degree of integration of non-dispensing pharmacists in primary care practice and the impact on health outcomes: a systematic review. Res Soc Adm Pharm. 2018;14:228–40.
Weber ZA, Skelley J, Sachdev G, et al. Integration of pharmacists into team-based ambulatory care practice models. Am J Health Syst Pharm. 2015;72(9):745–51. https://doi.org/10.2146/ajhp140576.
Benson H, Lucas C, Benrimoj SI, Williams KA. The development of a role description and competency map for pharmacists in an interprofessional care setting. Int J Clin Pharm. 2019;41(2):391–407. https://doi.org/10.1007/s11096-019-00808-4.
Benson H, Lucas C, Kmet W, Benrimoj SI, Williams K. Pharmacists in general practice: a focus on drug-related problems. Int J Clin Pharm. 2018;40(3):566–72. https://doi.org/10.1007/s11096-018-0617-9.
Hayhoe B, Cespedes JA, Foley K, Majeed A, Ruzangi J, Greenfield G. Impact of integrating pharmacists into primary care teams on health systems indicators: a systematic review. Br J Gen Pract. 2019;69:e665–74.
Stuhec M, Lah L. Clinical pharmacist interventions in elderly patients with mental disorders in primary care focused on psychotropics: a retrospective pre-post observational study. Ther Adv Psychopharmacol. 2021;11:20451253211011007.
Stuhec M, Gorenc K, Zelko E. Evaluation of a collaborative care approach between general practitioners and clinical pharmacists in primary care community settings in elderly patients on polypharmacy in Slovenia: a cohort retrospective study reveals positive evidence for implementation. BMC Health Serv Res. 2019;19(1):118.
Stuhec M, Flegar I, Zelko E, Kovačič A, Zabavnik V. Clinical pharmacist interventions in cardiovascular disease pharmacotherapy in elderly patients on excessive polypharmacy: a retrospective pre-post observational multicentric study. Wien Klin Wochenschr. 2021;133(15-16):770–9.
Stuhec M, Gorenc K. Positive impact of clinical pharmacist interventions on antipsychotic use in patients on excessive polypharmacy evidenced in a retrospective cohort study. Global Psychiatry. 2019;2:155–63. https://doi.org/10.2478/gp-2019-0013.
NHS England, Public Health England, Health Education England, Monitor, Care Quality Commission, NHS Trust Development Authority. Five year forward view. http://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf. Accessed 18 Aug 2020.
Mann C, Anderson C, Avery A, Waring J, Boyd M. Clinical pharmacists in general practice: pilot scheme independent evaluation report: full report: University of Nottingham; 2018. https://www.nottingham.ac.uk/pharmacy/documents/generalpracticeyearfwdrev/clinical-pharmacists-in-general-practice-pilot-scheme-full-report.pdf. Accessed 13 Jan 2020.
Reiss-Brennan B, Brunisholz KD, Dredge C, Briot P, Grazier K, Wilcox A, et al. Association of integrated team-based care with health care quality, utilization, and cost. JAMA. 2016;316:826–34.
Weeks G, George J, MacLure K, Stewart D. Non-medical pre-scribing versus medical prescribing for acute and chronic disease management in primary and secondary care. Cochrane Database Syst Rev. 2016;11:CD01122.
Anderson C, Zhan K, Boyd M, Mann C. The role of pharmacists in general practice: a realist review. Res Soc Adm Pharm. 2019;15:338–45. https://doi.org/10.1016/j.sapharm.2018.06.001.
Raynsford J, Dada C, Stansfield D, Cullen T. Impact of a specialist mental health pharmacy team on medicines optimisation in primary care for patients on a severe mental illness register: a pilot study. Eur J Hosp Pharm. 2020;27(1):31–5.
Nkansah N, Mostovetsky O, Yu C, Chheng T, Beney J, Bond CM, et al. Effect of outpatient pharmacists’ non-dispensing roles on patient outcomes and prescribing patterns. Cochrane Database Syst Rev. 2010;2010(7):CD000336. https://doi.org/10.1002/14651858.CD000336.pub2.
Trust GPs to lead: learning from the response to COVID-19 within general practice in England BMA. 2020. Available from: https://www.bma.org.uk/media/2652/bma-report-trust-gps-to-lead-june-2020.pdf. Accessed 01 Sep 2020.
Avery AJ. Pharmacists working in general practice: can they help tackle the current workload crisis? Br J Gen Pract. 2017;67(662):390–1.
Jorgenson D, Laubscher T, Lyons B, Palmer R. Integrating pharmacists into primary care teams: barriers and facilitators. Int J Pharm Pract. 2014;22(4):292–9. https://doi.org/10.1111/ijpp.12080.
Schlosser RW, Sigafoos J. ‘Empty’ reviews and evidence-based practice. Evid Based Commun Assess Interv. 2009;1–3. https://doi.org/10.1080/17489530902801067.
Acknowledgements
The authors would like to thank Andrew Doyle, library specialist at Aston University, for his guidance with the development of the search strategy.
Funding
None.
Author information
Authors and Affiliations
Contributions
NI was responsible for the data collection and contributed to the analysis, synthesis, interpretation and project management. He led the drafting of this article. CH provided methodological, analysis and synthesis input and contributed to the data collection and synthesis. In case any disagreement occurred, the final decision was made by a discussion with IM and the systematic reviewer (NI/CH) to reach an amicable solution. No concerns were raised. IM contributed to the analysis. NI designed and conducted the searches with support from CH and contributed to data collection. All authors contributed to revised successive drafts of this article and approved the final version submitted for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors agree with the publication of this article.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: S1.
List of Search Terms.
Additional file 2: S2.
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist.
Additional file 3: S3.
PRISMA 2020 for Abstracts Checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Iqbal, N., Huynh, C. & Maidment, I. Systematic literature review of pharmacists in general practice in supporting the implementation of shared care agreements in primary care. Syst Rev 11, 88 (2022). https://doi.org/10.1186/s13643-022-01933-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-022-01933-4